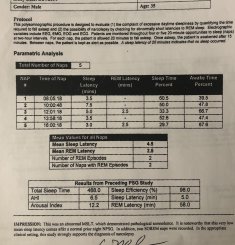
Has anyone ever had any success getting that condition rated by DOD at a PEB? Apparently, my sleep apena is causing or contributing to hypersomnia during the day. I have 2 or more episodes of interrupted sleep at night. Been on CPAP since 2014 with not real improvement. Have had 2 MSLT’s - ins strong for narcolepsy diagnosis, the other possible narcolepsy but probably hypersomnia.
I thought I might have narcolepsy, but the doctor says the wake ups make him think otherwise...
I thought I might have narcolepsy, but the doctor says the wake ups make him think otherwise...